Children across the United States require quality health insurance for proper development. The Children’s Health Insurance Program provides essential coverage like well-child visits and dental benefits to help low-income families cover an uninsured child. This health insurance program runs jointly with state Medicaid to assist families without private coverage.
9 Services Covered by CHIP
- Emergency Services
- Prescriptions
- Doctor Visits
- Inpatient and Outpatient Hospital Care
- Dental and Vision Care
- Routine Check-Ups
- Laboratory and X-ray Services
- Immunizations
- Behavioral Health Care
Private health insurance is a benefit that many American families don’t have, either because their job doesn’t offer it or because they can’t afford it on their own. To ensure that Americans have access to quality healthcare, the federal government offers programs like Medicare and Medicaid.
The Children’s Health Insurance Program (CHIP) targets children whose family income makes them ineligible for Medicaid services. Generally, children can qualify for CHIP even if their family’s income is 140% of the Federal Poverty Level (FPL). Some states allow incomes as high as 324% of the FPL, allowing health benefits to reach families who need them most.
What Is CHIP?
The Children’s Health Insurance Program provides comprehensive health insurance to children who do not otherwise qualify for Medicaid coverage due to income limits. The Centers for Medicare and Medicaid Services (CMS) manages this federal government health insurance program as well as Medicaid, Medicare, and the Health Insurance Marketplace.
The primary goal of CHIP is to include families with children in low-cost health coverage that children need for healthy development. Many families that qualify for CHIP have incomes that are higher than the threshold to qualify for Medicaid, food stamps, and other federal benefits but are still within a specific range of the Federal Poverty Level.
In 2020, more than nine million children were enrolled in the CHIP program within their state, with Texas, New York, and California having among the highest number of enrollees. This is only about 25% of the more than 35 million children enrolled in Medicaid in 2020. This is partly due to the several states that have implemented Medicaid expansion coverage through the Affordable Care Act, allowing more families to qualify for Medicaid with higher incomes.
Although CHIP is a federal health insurance program, each state manages its own CHIP program. This allows states to decide income limits for their program based on the Federal Poverty Level, average family income, and cost of living for areas within the state.
States can choose to add optional care services to their CHIP plans, but every state must include four mandatory coverages in their CHIP health plan. Dental benefits, well-baby and well-child visits, vaccinations, and behavioral health are mandatory coverages through CHIP that each state includes.
Other states extend coverage to pregnant women to offer maternity-related medical care. Some children can also get vision insurance, emergency care benefits, and prescription drug coverage through their state’s program.
While some CHIP benefits are free to many families, others could require copays or coinsurance. Some states participate in cost-sharing, which requires families to pay specific amounts for services or meet low-cost deductibles before their CHIP plan begins paying.
Who Is Eligible for CHIP?
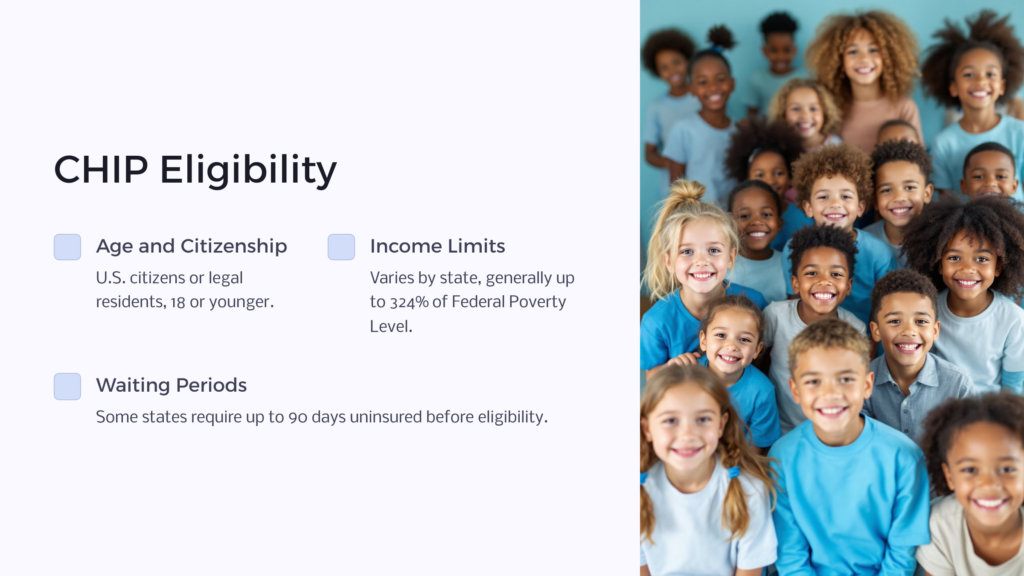
CHIP eligibility varies by state. However, the federal health insurance program does make some eligibility guidelines nationwide, including being a U.S. citizen and having proof of your legal status. Children must also be 18 or younger to qualify.
Recipients must also qualify by income, but income limits are different in each state and county within a state due to cost of living, average incomes, and other factors. Generally, the income guidelines for CHIP are more forgiving than those to qualify for Medicaid services, as CHIP is designed to cover families who may be slightly over the income limits for Medicaid.
Some states, including Florida, Iowa, and New Jersey, vary their income limits based on federal poverty levels.
Another variation between states regarding eligibility is the waiting period for families before becoming eligible for the Children’s Health Insurance Program. This waiting period is the time families must be uninsured before they qualify for CHIP. CHIP does not allow the waiting period to stretch longer than 90 days, but Maine, Texas, and Illinois are among the few states that require families to wait the full waiting period.
Other states, like Iowa and Florida, require only 60 days, while Wyoming has a 30-day waiting period.
Some states do have exceptions to their waiting periods. For instance, babies younger than one can qualify with no waiting period in Illinois, and victims of domestic violence do not need to wait to enroll in Florida.
In some areas, pregnant women may also qualify for CHIP. Currently, South Dakota, Oregon, and Arkansas are a few states that extend coverage to pregnant women who meet income and other eligibility guidelines. Comprehensive and prenatal care are included in some states, but others extend only prenatal care coverage.
You can check your state’s CHIP eligibility guidelines through its benefits or Medicaid website or via InsureKidsNow.gov.
How To Apply for CHIP
If you’ve applied for Medicaid coverage, your application would have also been submitted for potential CHIP insurance coverage. Your local benefits agency will review your documentation and application and decide whether your income qualifies you for Medicaid or CHIP.
However, you can also apply for CHIP separately if you believe you or your child will not qualify for Medicaid based on your local income limit guidelines. To do this, you can call the Health Insurance Marketplace at 1-800-318-2596 or fill out an online application at Healthcare.gov. Based on your income, the Marketplace will determine whether you might qualify and send your information to your local Medicaid/CHIP agency for further approval.
You can also apply at your local agency if you prefer. InsureKidsNow.gov also makes it easy to find out where to apply for CHIP in your state.
When applying for CHIP, you’ll need information about you and everyone living in your household, including names, birth dates, and Social Security numbers. Also, include proof of residency, proof of employment, and proof of income. You may also need documentation to show unearned income, like investments and child support payments. Some household members may require documentation proving their relationships to you, like an adopted child or a spouse.
9 Services Covered by CHIP

The Children’s Health Insurance Program differs between states. Still, several services don’t have mandatory insurance coverage, but most states still elect to include them in CHIP coverage. Eligible children can usually receive the following covered services under CHIP:
1. Emergency Services
Emergency services coverage under CHIP isn’t mandatory, but most states choose to cover them, including urgent care visits, emergency room visits, and ambulatory transportation. This coverage may also include x-rays, diagnostic tests, lab work, and other tests that can diagnose emergency problems.
2. Prescriptions
Prescription coverage is also not mandatory but is included in each state’s CHIP program as part of its mission to provide comprehensive health coverage for children. Many prescriptions allowed through CHIP are free to families, while others have small co-pays. In many cases, parents and caregivers can work with their child’s doctor to prescribe generic forms of prescription medications that CHIP will cover for little to no out-of-pocket costs.
3. Doctor Visits
Doctor visits that don’t follow routine well-baby and well-child checkup schedules are usually covered by state CHIP programs. Children might visit the doctor with a new health concern, when they’re sick, or when they need a physical. These visits are essential parts of a child health profile, so health care coverage for them is necessary for families with limited income.
4. Inpatient and Outpatient Hospital Care
When a child needs services at a hospital as an inpatient or outpatient, CHIP may provide coverage. Examples of inpatient services include a hospital stay, surgery, or mental or behavioral health monitoring. Outpatient services may include outpatient surgery, physical therapy visits, or chemotherapy treatments. These often high-cost services can become more affordable for CHIP-eligible families who need them.
5. Dental and Vision Care
Dental services are mandatory through CHIP but vision care is not. Still, many states include CHIP benefits for both, ensuring that eligible children get routine dental and vision care. Services may cover teeth cleanings and exams, basic dental procedures, a pair of eyeglasses, and an annual eye exam.
6. Routine Check-Ups
Routine well-baby and well-child visits must be covered by every state’s Children’s Health Insurance Program. These necessary doctor visits monitor critical developmental milestones in children of all ages and can help prevent and diagnose any potential health problems. They can also help primary care physicians decide whether referrals to specialists are necessary.
7. Laboratory and X-ray Services
An uninsured child with CHIP health insurance coverage can typically get lab services and x-ray services covered by their state’s CHIP plan. These services assist medical professionals with diagnosing conditions and treating them in a child and are, therefore, a crucial part of the child’s health care.
8. Immunizations
Each state’s CHIP program must cover immunizations. Any vaccines that are mandatory for a baby or child will have coverage through CHIP.
9. Behavioral Health Care
Behavioral health care services also have mandatory coverage in each state. This coverage can ensure that children are following healthy cognitive, social, emotional, and mental development. Covered services may include therapy, psychiatry, psychology, inpatient stays for diagnostics or treatment, or social work services.
How Much Does CHIP Cost?
The Children’s Health Insurance Program makes healthcare services more affordable for families with children or pregnant women. Depending on the state in which they reside, some families will need to pay premiums or copays for specific services. Other states do not require families to pay anything for CHIP services, including Ohio, New York, and South Dakota.
States can determine what services families need to pay for and how much they pay for those services. However, CHIP guidelines require states to charge no more than 5% of an eligible family’s income for CHIP services.
Some states have families pay premiums, which are monthly or annual payments they make to remain in the program. Other states require them to pay a copay, which is a specific dollar amount or percentage of the cost of the service.
Here are a few examples of states that require copays or premiums:
- Wisconsin charges CHIP families a $3 maximum copay each time they use a physician, outpatient, or inpatient service. They also pay $10-$98/month per child.
- Pennsylvania requires some families to pay up to a $15 copay for outpatient and physician services and up to $50 for inpatient services or ER visits, but the lowest-income families on CHIP do not pay for these services. Higher-income families pay monthly premiums between $53-$74.
- Illinois charges an annual premium for each child for families in its higher-income plans, but no family pays more than $80/month.
- Wyoming offers three CHIP plans with copays ranging from $0-$50.
It’s important to note that well-baby, well-child, and dental services are always free through CHIP, regardless of the state you live in. Additionally, CHIP exempts Native Americans and Alaska Natives from paying any copays, premiums, or other out-of-pocket costs.
Children’s Health Insurance Program
The Children’s Health Insurance Program from the federal government allows states to provide comprehensive health coverage to families with children or pregnant women who do not qualify for Medicaid. The higher income limits for CHIP extend Medicaid coverage to families who need affordable health insurance.
While states can decide the specifics of their CHIP health plan or plans, the government requires all states to provide basic medical care under CHIP, including dental services and well-child checkups. Other services may be covered depending on the state, but some families could have to pay copays or premiums for those services.
When you apply for Medicaid, your family will automatically be considered for CHIP, too. You can also apply for CHIP separately through your local benefits office or by visiting InsureKidsNow.gov.
 Benefits.com Advisors
Benefits.com Advisors
With expertise spanning local, state, and federal benefit programs, our team is dedicated to guiding individuals towards the perfect program tailored to their unique circumstances.
Rise to the top with Peak Benefits!
Join our Peak Benefits Newsletter for the latest news, resources, and offers on all things government benefits.