Sciatica is a common and often painful condition that affects the sciatic nerve, which is the largest nerve in the human body. It typically originates in the lower back and extends down into the leg. For veterans, sciatica can be a particularly challenging condition due to the physical demands and rigorous training associated with military service.
Sciatica is characterized by symptoms such as sharp, shooting pain, tingling, numbness, and muscle weakness in the lower back, buttock, and leg. These symptoms can vary in intensity and may be exacerbated by physical activity or prolonged periods of sitting.
Military service often puts veterans at risk for developing sciatica. Factors such as heavy lifting, extended periods of standing or sitting, and physically demanding training exercises can contribute to the development or exacerbation of sciatic nerve damage. Additionally, service-related injuries or conditions, such as herniated discs or spinal injuries, can increase the likelihood of sciatica pain among veterans.
Understanding sciatica and its impact on veterans is crucial for those navigating the VA disability system. By recognizing the symptoms and risk factors associated with sciatica, veterans can better advocate for themselves when seeking disability benefits from the VA. In the following sections, we will delve deeper into the VA’s disability rating system and the process of applying for sciatica-related benefits.
What is Sciatic Nerve Pain?

Sciatic nerve pain, commonly known as sciatica, is a debilitating condition. It originates from the compression or irritation of the sciatic nerve, the longest nerve in the body. This nerve runs from the lower back, down through the buttocks, and extends into each leg. When the sciatic nerve is compressed or inflamed, it leads to a range of distressing symptoms. This level of pain can significantly impact a person’s daily life. This is especially true for veterans, who have experienced demanding service.
The hallmark symptom of sciatica is a sharp, shooting pain that radiates along the path of the sciatic nerve. This pain often starts in the lower back and can travel down through the buttocks and the back of one or both legs. The intensity of the pain can vary from mild to incapacitating. Alongside the pain, veterans with sciatica might also experience:
- Numbness and Tingling: The compression of the sciatic nerve can lead to tingling, or a “pins and needles” feeling in the buttocks, legs, and feet.
- Muscle Weakness: Sciatica can cause weakness in the muscles of the affected leg, making it difficult to perform routine activities such as walking, standing, or climbing stairs.
- Limited Mobility: The combination of pain, numbness, and muscle weakness can severely restrict a veteran’s range of motion, making even basic movements a challenge.
- Impact on Quality of Life: The chronic pain and limitations associated with sciatica can significantly affect a veteran’s overall well-being, interfering with their ability to work, engage in recreational activities, and enjoy daily life.
Veterans may be at an increased risk of developing sciatica due to factors such as heavy lifting, repetitive motions, and exposure to challenging environments. Sciatica can pose not only physical but psychological and financial challenges. Veterans may find that it hinders their work and livelihood, which is just as discouraging as physical pain.

The complexities of sciatica make it difficult to veterans to ask for help. The appropriate compensation and support for their condition may vary case to case. By recognizing the range of symptoms, potential causes, and impact on daily life, veterans can effectively communicate their challenges. This is vital for a successful social security application. Accurate documentation of symptoms, medical records, and expert evaluations will help. Be thorough when seeking compensation for sciatica’s impact on your life.
VA Disability Rating for Sciatica: How is it Assessed?
The VA evaluates disabilities by assigning ratings. These quantify the severity of a condition’s impact on an individual’s daily life. Sciatica’s disability rating is based on the extent of pain, functional limitations, and impact on veterans’ ability to work. Ratings can range from 0% to 100%. The higher the rating, the greater the compensation veterans may be eligible for. For veterans seeking compensation for sciatica, the assigned disability rating determines their financial support and access to medical care.
Benefits Available to Veterans with Sciatica

Veterans impacted by sciatica can access various benefits to aid in managing their condition:
- Financial Aid: Disability compensation offers support proportional to the assigned rating, and helps veterans cope with physical and financial implications of their condition.
- Medical Care: VA healthcare services provide veterans with comprehensive medical evaluations, treatment plans, and therapies to alleviate sciatic nerve pain and improve overall well-being.
- Vocational Rehabilitation: For veterans whose sciatica hampers their ability to work, vocational rehabilitation services offer opportunities to develop new skills and explore alternative career paths.
Navigating Sciatica’s Connection to Service and SSDI Eligibility: Documentation Matters
Understanding whether sciatica is service-connected and qualifying for Social Security Disability Insurance (SSDI) benefits is a two-fold issue. It involves assessing both the VA and SSA criteria. While the VA focuses on service-related disabilities, the SSA takes a broader approach, evaluating an individual’s overall ability to work.
Is Sciatica Service-Connected?
In terms of VA benefits, establishing service-connection for sciatica can be complex. To qualify for VA disability compensation, veterans must prove a direct link between their military service and the development of sciatica. Proving that service-related factors, such as physically demanding tasks or exposure to hazardous conditions, directly contributed to the onset or worsening of sciatica is crucial. Additionally, veterans need to provide documented medical evidence, such as diagnosis records, treatment history, and expert opinions, to support their claim. While proving service connection for sciatica may pose challenges, it’s not impossible. Comprehensive documentation and expert assessments can strengthen a veteran’s case for service connection, especially if they can establish a clear connection between their military duties and the development of sciatica.
SSI vs. SSDI: The Difficulty of SSDI Approval for Sciatica
When it comes to Social Security Disability Insurance (SSDI), the approval process can be rigorous, and sciatica’s status as a qualifying disability may be influenced by several factors:
- Severity of Impairment: SSDI requires a disability to be severe enough to significantly limit the individual’s ability to work. While sciatica’s impact can vary, veterans with severe symptoms that impede substantial work may have a better chance of approval.
- Substantial Gainful Activity (SGA): SSDI considers the applicant’s ability to engage in SGA, which involves earning a certain income through work. If sciatica prevents a veteran from earning above the SGA threshold due to limitations on physical activity, their chances of approval increase.
Documentation that Strengthens the Case
To enhance the likelihood of SSDI approval for sciatica, comprehensive documentation is essential:
- Medical Records: Detailed medical records, including diagnosis, treatment history, and expert assessments, provide substantial evidence of the condition’s severity and impact on daily life.
- Functional Limitations: Clearly documented functional limitations resulting from sciatica, such as restricted mobility, inability to stand or sit for extended periods, and difficulty performing basic tasks, can illustrate how the condition affects a veteran’s ability to work.
- Treatment Records: Consistent and thorough treatment records showcase the veteran’s commitment to managing their condition and their willingness to follow medical recommendations.
- Expert Opinions: Expert medical opinions, especially those from specialists who can detail the nature and extent of the disability, can carry significant weight in the SSA’s evaluation.
So while sciatica’s service connection with military duties may be intricate to establish, its recognition as a qualifying disability for SSDI involves demonstrating the severity of functional limitations and their impact on substantial gainful activity. Documentation, ranging from medical records to expert opinions, plays a crucial role in presenting a comprehensive case to both the VA and SSA.
For veterans seeking compensation and support for their sciatica-related challenges, diligent gathering and presentation of evidence are key in securing the benefits they rightfully deserve.
Navigating the Application Process
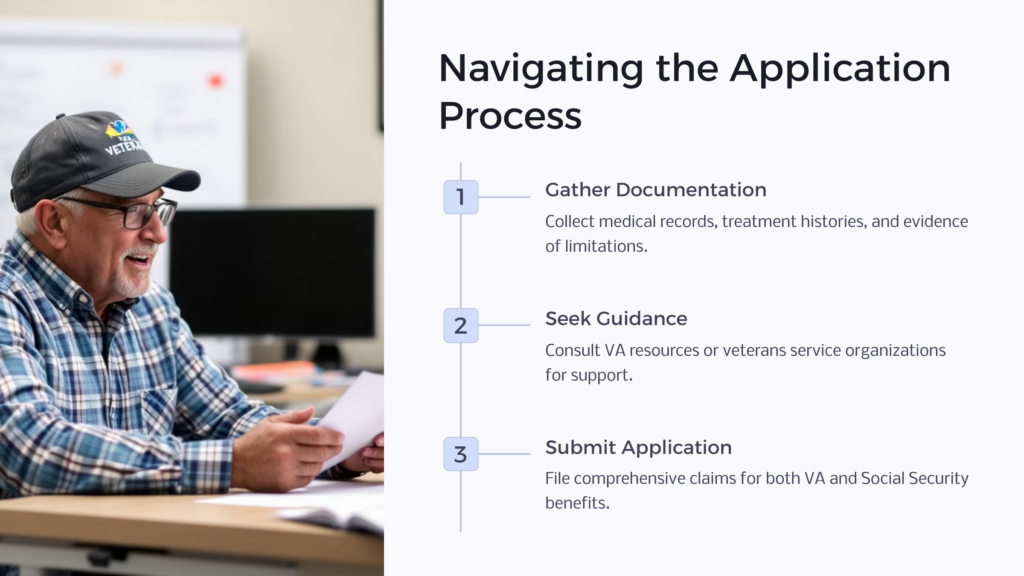
Successful chances of application for both VA disability benefits and Social Security disability benefits require careful planning. Gather medical records, treatment histories, and documentation of functional limitations related to sciatica. Consult VA resources or veterans service organizations for guidance and support.
When seeking Social Security benefits, it’s important to realize that sciatica’s impact on work is a central consideration. So, ensure to gather comprehensive medical documentation that outlines the condition’s severity, functional limitations, and treatment history. Seek assistance from experts to ensure a well-prepared application.
For veterans grappling with sciatica, this knowledge empowers them to navigate both the VA and Social Security processes. By seeking proper guidance and assembling compelling evidence, veterans can secure the financial and medical support they deserve while managing the impact of sciatica on their lives. Contact us today to see how our experts can help you!
 Benefits.com Advisors
Benefits.com Advisors
With expertise spanning local, state, and federal benefit programs, our team is dedicated to guiding individuals towards the perfect program tailored to their unique circumstances.
Rise to the top with Peak Benefits!
Join our Peak Benefits Newsletter for the latest news, resources, and offers on all things government benefits.



















