Diverticulitis and diverticulosis are two related conditions that affect the digestive system, particularly the colon. Understanding these conditions is crucial for veterans seeking VA disability benefits for diverticulitis.
Diverticulosis occurs when small, bulging pouches (diverticula) form in the lining of the digestive tract, most commonly in the colon. These pouches are usually harmless and may not cause any symptoms. Many people with diverticulosis don’t even know they have it.
Diverticulitis, on the other hand, happens when these pouches become inflamed or infected. This condition can cause severe abdominal pain, fever, nausea, and changes in bowel habits. Diverticulitis can be acute (short-term) or chronic (long-term) and may require medical treatment or even surgery in severe cases.
Understanding the Symptoms and Causes of Diverticulitis
The symptoms of diverticulitis can vary from person to person, but common signs include:
- Sharp pain in the lower left abdomen
- Fever and chills
- Nausea and vomiting
- Changes in bowel habits (constipation or diarrhea)
- Bloating and gas
- Rectal bleeding (in some cases)
The exact cause of diverticulitis is not fully understood, but several factors may contribute to its development:
1. Low-fiber diet: A diet low in fiber can lead to constipation and increased pressure in the colon, which may cause diverticula to form.
2. Age: The risk of developing diverticulitis increases with age, especially after 40.
3. Obesity: Being overweight or obese can increase the risk of diverticulitis.
4. Lack of exercise: A sedentary lifestyle may contribute to the development of diverticulitis.
5. Smoking: Tobacco use has been linked to an increased risk of diverticulitis.
For veterans, stress and certain medications may also play a role in developing or exacerbating diverticulitis symptoms. This is particularly important when considering a VA claim for diverticulitis or exploring the possibility of diverticulitis secondary to PTSD.
How Diverticulitis is Diagnosed and Treated
Diagnosing diverticulitis typically involves a combination of physical examination, medical history review, and diagnostic tests. Common diagnostic procedures include:
- CT scan: This imaging test can show inflamed or infected pouches and the severity of the condition.
- Colonoscopy: While not usually performed during acute episodes, a colonoscopy may be recommended after symptoms subside to evaluate the colon.
- Blood tests: These can help detect signs of infection or inflammation.
Treatment for diverticulitis depends on the severity of the condition. Mild cases may be treated with:
- Antibiotics to clear the infection
- A liquid or low-fiber diet to allow the colon to heal
- Pain medications to manage discomfort
Severe cases or those with complications may require:
- Hospitalization for intravenous antibiotics and fluids
- Surgery to remove the affected part of the colon
- Drainage of abscesses if they form
For veterans seeking VA compensation for diverticulitis, proper documentation of diagnosis and treatment is crucial in supporting their claim.
Service Connection for Diverticulitis in Veterans
To receive VA disability benefits for diverticulitis, veterans must establish a service connection. This means proving that their condition is related to their military service. There are three main ways to establish service connection:
1. Direct service connection: The veteran can show that their diverticulitis began during or was caused by their military service.
2. Secondary service connection: If the veteran’s diverticulitis is caused or aggravated by another service-connected condition (such as PTSD), they may be eligible for benefits.
3. Presumptive service connection: In some cases, the VA presumes certain conditions are related to military service, though diverticulitis is not currently on this list.
To support a claim for service connection, veterans should gather:
- Service medical records showing diagnosis or treatment of diverticulitis or related symptoms
- Post-service medical records documenting ongoing issues with diverticulitis
- Statements from fellow service members or family members who can attest to the onset or progression of symptoms
- Medical opinions linking the condition to military service or a service-connected disability
Veterans exploring the possibility of diverticulitis secondary to PTSD should work closely with their healthcare providers to establish a clear link between the two conditions.
Navigating the VA Claims Process for Diverticulitis
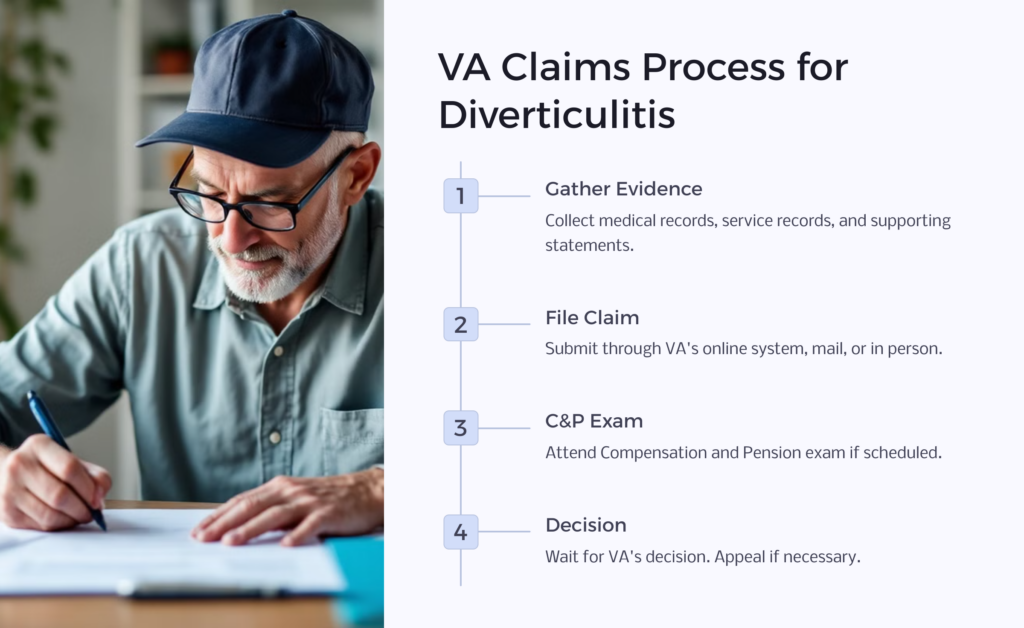
Filing a VA claim for diverticulitis can be complex, but understanding the process can help veterans navigate it more effectively:
1. Gather evidence: Collect all medical records, service records, and supporting statements related to your diverticulitis.
2. File the claim: Submit a claim through the VA’s online system, by mail, or in person at a VA office. Be sure to specifically claim diverticulitis and any related symptoms.
3. Attend C&P exam: The VA may schedule a Compensation and Pension (C&P) exam to assess the severity of your condition. Be honest and thorough about your symptoms and how they affect your daily life.
4. Wait for a decision: The VA will review your claim and issue a decision. This process can take several months.
5. Appeal if necessary: If your claim is denied or you disagree with the rating, you have the right to appeal the decision.
Throughout this process, it’s important to be proactive and keep copies of all documents submitted to the VA. Veterans may also consider seeking assistance from a Veterans Service Organization (VSO) or a VA-accredited attorney to help with their claim.
Diverticulitis VA Disability Ratings Explained
The VA rates diverticulitis under 38 CFR § 4.114, Diagnostic Code 7327. This code directs the VA to rate the condition as irritable bowel syndrome, peritoneal adhesions, or ulcerative colitis, depending on the predominant disability picture.
Ratings can range from 0% to 100%, depending on the severity of symptoms:
- 0%: Mild symptoms that can be controlled by diet
- 10%: Moderate symptoms with frequent episodes of bowel disturbance and abdominal distress
- 30%: Severe symptoms with diarrhea or alternating diarrhea and constipation, with more or less constant abdominal distress
- Higher ratings (up to 100%) may be assigned for severe complications such as malnutrition, liver abscess, or total disability
It’s important to note that the VA will assign a single evaluation under the diagnostic code that reflects the predominant disability picture. This means that even if a veteran has symptoms that could fall under multiple diagnostic codes, they will typically receive only one rating for their gastrointestinal condition.
Veterans should be aware that their VA rating for diverticulitis symptoms may change over time if their condition improves or worsens. Regular medical check-ups and documentation of symptoms can help ensure that the VA rating accurately reflects the current severity of the condition.
Common Challenges in Securing Diverticulitis VA Ratings
Veterans often face several challenges when seeking VA disability ratings for diverticulitis:
1. Lack of in-service documentation: If symptoms began after service or were not well-documented during service, it can be difficult to establish a direct service connection.
2. Overlapping symptoms: Diverticulitis symptoms can overlap with other gastrointestinal conditions, making it challenging to get an accurate diagnosis and rating.
3. Intermittent nature of symptoms: Because diverticulitis can flare up and then subside, it may be hard to demonstrate the chronic nature of the condition.
4. Proving secondary connection: When claiming diverticulitis as secondary to another condition like PTSD, providing strong medical evidence of the link can be challenging.
To overcome these challenges, veterans should:
- Keep detailed records of all symptoms, treatments, and how the condition affects daily life
- Work closely with healthcare providers to get clear diagnoses and opinions on service connection
- Consider getting a second medical opinion if initial diagnoses are unclear
- Be prepared to explain how the condition impacts quality of life during C&P exams
Remember, persistence and thorough documentation are key when dealing with these common obstacles in the VA claims process.
How to Appeal a Denied Diverticulitis VA Claim
If your VA claim for diverticulitis is denied or you receive a lower rating than expected, you have the right to appeal the decision. Here’s how to navigate the appeals process:
1. Review the decision letter: Carefully read the VA’s explanation for their decision to understand why your claim was denied or rated lower than expected.
2. Choose your appeal lane: Under the new Appeals Modernization Act, you have three options:
3. Higher-Level Review: A senior VA employee reviews your existing claim
4. Supplemental Claim: You can submit new and relevant evidence
5. Appeal to the Board of Veterans’ Appeals: Your case is reviewed by a Veterans Law Judge
6. Gather additional evidence: If you choose the Supplemental Claim lane, collect any new medical records, lay statements, or expert opinions that support your case.
7. Submit your appeal: File the appropriate form for your chosen appeal lane within the specified timeframe (usually one year from the date of the decision).
8. Attend hearings if necessary: If you appealed to the Board, you may have the option to attend a hearing to present your case.
9. Wait for a new decision: The VA will review your appeal and issue a new decision. This process can take several months to over a year.
Throughout the appeals process, it’s crucial to stay organized, meet all deadlines, and consider seeking help from a VSO or VA-accredited attorney who specializes in VA disability claims.
The Role of Secondary Conditions in Diverticulitis Claims
Secondary service connection can be an important avenue for veterans seeking VA compensation for diverticulitis. This approach is particularly relevant when considering diverticulitis secondary to PTSD or other service-connected conditions.
To establish a secondary service connection, veterans must show:
1. They have a current diagnosis of diverticulitis
2. They have an existing service-connected condition (e.g., PTSD)
3. Medical evidence that their diverticulitis is caused or aggravated by the service-connected condition
Common secondary connections for diverticulitis include:
- Mental health conditions like PTSD or depression, which can exacerbate gastrointestinal issues
- Medications taken for service-connected conditions that may contribute to diverticulitis
- Service-connected conditions that lead to a sedentary lifestyle, increasing the risk of diverticulitis
When pursuing a secondary connection claim, it’s crucial to obtain a strong medical opinion that clearly explains the relationship between the primary service-connected condition and diverticulitis. This may involve working with both mental health professionals and gastroenterologists to build a comprehensive case.
Veterans should also be prepared to explain how their primary condition has impacted their diet, stress levels, or overall health in ways that contribute to diverticulitis. Detailed documentation of symptoms and their correlation with the primary condition can significantly strengthen a secondary claim.
Resources and Support for Veterans with Diverticulitis
Veterans dealing with diverticulitis have several resources available to help them manage their condition and navigate the VA claims process:
1. VA Health Care: Eligible veterans can receive treatment for diverticulitis through the VA healthcare system. This includes access to gastroenterologists, nutritionists, and other specialists.
2. Veterans Service Organizations (VSOs): Organizations like the Disabled American Veterans (DAV) and Veterans of Foreign Wars (VFW) offer free assistance with VA claims and appeals.
3. VA Vet Centers: These centers provide counseling services that can be helpful for veterans dealing with the stress of chronic health conditions.
4. Online Support Groups: Various online forums and social media groups connect veterans with diverticulitis, offering peer support and advice.
5. Nutritional Resources: The VA often provides nutritional counseling to help veterans manage their diet, which is crucial for controlling diverticulitis symptoms.
6. VA Caregiver Support: For veterans whose diverticulitis severely impacts their daily life, the VA offers support programs for caregivers.
7. Legal Aid: Some organizations provide pro bono legal assistance to veterans struggling with VA claims and appeals.
Veterans should also stay informed about any changes in VA policies or rating criteria that might affect their diverticulitis claims. Regularly checking the VA’s official website and consulting with VSOs can help veterans stay up-to-date on any developments that could impact their benefits.
Remember, managing diverticulitis is an ongoing process. By taking advantage of these resources and maintaining open communication with healthcare providers and VA representatives, veterans can better manage their condition and ensure they receive the support and compensation they deserve.
 Benefits.com Advisors
Benefits.com Advisors
With expertise spanning local, state, and federal benefit programs, our team is dedicated to guiding individuals towards the perfect program tailored to their unique circumstances.
Rise to the top with Peak Benefits!
Join our Peak Benefits Newsletter for the latest news, resources, and offers on all things government benefits.



















