What Is a Basic Health Program?

Under the Affordable Care Act, states have the option to develop Basic Health Programs that extend benefits to low-income residents who would otherwise qualify to purchase benefits through the marketplace. These residents generally earn too much money to qualify for Medicaid, but not more than 200% of the Federal Poverty Level. Basic health programs are designed at minimum to cover the following essential benefits, which are specified within the Affordable Care Act.
10 Essential Health Benefits
- Outpatient Care
- Emergency Services
- Hospitalization
- Mental Health and Addiction Services
- Prenatal and Postpartum Care
- Prescription Drugs
- Rehabilitative Services
- Lab Tests
- Preventative Services
- Pediatric Services
A Basic Health Program serves two purposes: to provide continuity of care for households whose income might go back and forth between being eligible for Medicaid, CHIP, or other programs, and to make more comprehensive and affordable coverage available to citizens. Basic health care programs are made possible through the Affordable Care Act, and states receive federal compensation for households enrolled in their respective programs.
What Is a Basic Health Program?
A Basic Health Program helps close the gap between state-level aid and health care marketplace plans. Part of their purpose is to reduce the number of enrollees who transition back and forth between Medicaid, CHIP, and marketplace health care plans.
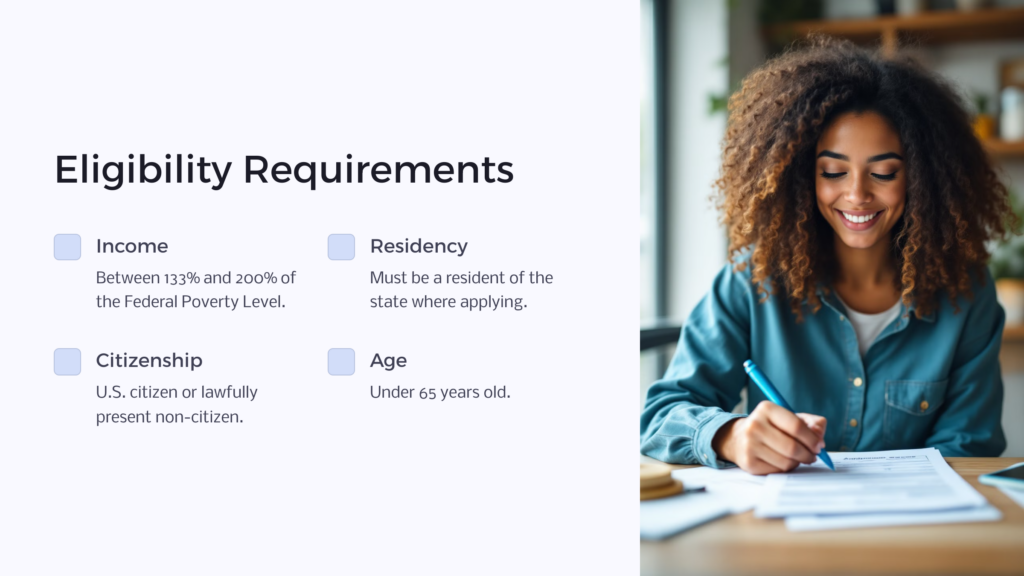
In states that facilitate these programs, a Basic Health Program is a low-cost health insurance coverage option for households that meet eligibility requirements. In general, applicants must meet the following requirements for enrollment to qualify for a basic health program:
- Have a household income between 133% – 200% of the Federal Poverty Level
- Be a resident of the state in which they are applying
- Be either a U.S. citizen or a lawfully present non-citizen
- Be younger than age 65
- Be ineligible for minimum essential coverage, which includes CHIP, Medicaid, and affordable employer-sponsored health insurance
- Not be incarcerated, besides during a period pending disposition of charges
Basic health programs are available that feature a wide variety of benefits, but at minimum, each basic health program a state offers must include coverage of the 10 essential services found in the Affordable Care Act, which are listed above. While states can choose to add more coverage options, they cannot offer fewer options.
Which States Use a Basic Health Program?
Basic health programs are currently in place in New York and Minnesota. Residents of these states now have access to more affordable health care coverage than they would if they lived in any of the other U.S. states. Developing this program for their states allows both New York and Minnesota to offer benefits to citizens that the states previously had funded on their own, but now with tremendous federal funding support.
Minnesota partners with seven different private insurers to offer MinnesotaCare, which by recent count boasts more than 87,000 members. Most people who are enrolled in the program pay premiums of between $16 and $80 per month. Native American residents who qualify pay no premiums at all.
New York’s Essential Plan features more than 800,000 enrollees, partnering with 16 private insurers across the state to provide BHP coverage. Depending on household income, those who have enrolled pay premiums of either $0 or $20. For those with no premiums, most copays vary from $1-$3, and other necessary medical services have no copays, deductibles, or coinsurance payments associated with them. For enrollees who pay the $20 premium, possible out-of-pocket costs might include $15 copays for branded drugs, $25 copays for specialist office visits, and $150 copays for inpatient hospitalizations.
Both New York and Minnesota are financially healthier after starting their basic health programs. While they previously had relied solely on state funds to help lower-income residents with health care expenses, they now have substantial federal funding to support their programs. Other U.S. states may move to establish similar programs in the future. A 2012 Health Affairs study showed that if all 50 states were to implement a Basic Health Program, approximately 1.8 million fewer adults would go back and forth between Medicaid and qualified health plans each year.
10 Essential Health Benefits
All plans offered in the Marketplace on healthcare.gov cover these 10 essential health benefits:
Outpatient Care
Also known as ambulatory care, this category of benefits covers any medical care received on an outpatient basis, with no overnight stay in the hospital. After the procedure, the patient is free to leave the medical facility and recover at home.
Emergency Services
This category generally describes medical services received at a hospital emergency room. These services generally help diagnose and stabilize a medical condition with sudden onset and severity. In these situations, patients are not penalized if they get emergency care from an out-of-network provider.
Hospitalization
This covers medical services you receive as an inpatient in a hospital setting. BHP coverage may vary when it comes to extended hospital stays, but some costs associated with hospital care must be covered.
Mental Health and Addiction Services
Mental health and addiction services include counseling and other related services designed to help patients with behavioral health, up to and including psychotherapy.
Prenatal and Postpartum Care
Plans must cover services that ensure appropriate health care for mothers during and immediately after their pregnancies, along with providing newborn care.
Prescription Drugs
The ACA stipulates several categories of prescription drugs – at minimum, a health plan must cover one drug from each category, though it may cover more.
Rehabilitative Services
Services covered under this category are those that help an enrollee recover from injury or that help manage a disability or chronic condition. Examples might include occupational or physical therapy or speech therapy.
Lab Tests

Any test designed to help diagnose an illness or condition or to gauge the effectiveness of treatment should be covered under this category, along with some preventative screening services.
Preventative Services
In addition to yearly wellness visits, preventative services include activities associated with management of chronic diseases, such as Type 2 diabetes screenings, colorectal cancer screening, immunizations, vaccinations, and diet counseling.
Pediatric Services
Covered services include well-child visits, dental and vision care, immunizations, and vaccinations. Vision and dental care comprising two routine dental cleanings and one yearly visual assessment and corrective lenses must be included.
How Does the Basic Health Program Work?

To create a Basic Health Plan, the state partners with a group of private insurance companies to offer low-cost health coverage to qualified citizens. The premiums are intentionally set at affordable levels, and those who earn incomes up to 150% of the Federal Poverty Level are covered at a platinum level; those with income between 150% – 200% of the Federal Poverty Level are covered at a gold level. Qualifying residents receive health care coverage that not only is affordable but also robust and comprehensive.
Platinum level plans generally cover around 90% of a patient’s health care costs. The other 10% is expected to be paid by the enrollee in the form of copays, deductibles, or coinsurance. A gold health plan will generally cover 80% of the patient’s expenses, while the enrollee is responsible for the remaining 20%.
Much like Medicaid and other similar programs, qualified applicants can enroll anytime during the year.
For states that don’t have a Basic Health Program, their residents earning incomes between that state’s Medicaid eligibility cutoff and 200% of the Federal Poverty Level have the option to purchase premium subsidies and cost-sharing reductions if they buy health coverage in the exchange. This applies as long as they aren’t eligible for an employer-sponsored health plan and/or Medicare.
If a state chooses to develop a Basic Health Program, the federal government will pay that state an amount equal to 95% of the amount it would otherwise have spent on premium subsidies and cost-sharing reductions for the state’s residents who end up qualifying for the Basic Health Program. This allows the state to combine both federal and state funding to power its program.
Who Qualifies for a Basic Health Program?
The goal of a Basic Health Program is to help make health care affordable and accessible for those with low incomes, but who may earn too much to qualify for Medicaid, CHIP, or other state assistance programs. Those who enroll also must meet the eligibility requirements listed above. Generally, this means that those who earn between 138% – 200% of the Federal Poverty Level are eligible as long as they meet the other requirements.
Qualifying groups also may include lower-income residents who are ineligible for the Medicaid program because of their immigration status. It’s also important to note that the Basic Health Program has no asset requirements – income is the sole qualifying financial factor.
For residents who don’t qualify for a Basic Health Program policy, ACA-compliant coverage plans still are available through the healthcare marketplace. There may still be affordable plans available that can help cover medical costs, even though they will come at a higher premium than plans offered under a state’s Basic Health Program. The important thing is to make sure residents have some level of health care coverage in place to help avoid catastrophic medical costs.
Lower cost, ACA-compliant options may include the lowest-priced bronze individual or family health plan available in a specific area. Healthy individuals under age 30 also may be eligible for catastrophic coverage plans. These plans offer high-deductible, low premium coverage that meets all ACA criteria for essential coverage.
Basic Health Programs
Health insurance options can be varied and confusing when you consider Medicaid, CHIP, Medicare vs. Medicaid, the health care marketplace, state vs. federal options, and more. But just keep in mind that the Basic Health Program is designed to help patients who earn too much to qualify for Medicaid or similar programs, yet do not have income robust enough for them to afford the high premiums, co-pays, and other out-of-pocket costs in a standard health care plan. For states who choose to implement Basic Health programs, health care is expanded and more affordable to those in need.
 Benefits.com Advisors
Benefits.com Advisors
With expertise spanning local, state, and federal benefit programs, our team is dedicated to guiding individuals towards the perfect program tailored to their unique circumstances.
Rise to the top with Peak Benefits!
Join our Peak Benefits Newsletter for the latest news, resources, and offers on all things government benefits.



















